There is a significant connection between heart disease and Alzheimer’s disease, according to findings published in the Journal of the American Medical Association.
Researchers concluded, “arterial stiffness is strongly associated with the progressive deposition of Aβ in the brain.” Aβ, or beta amyloid, has long been studied as a cause of the degeneration of brain tissue in Alzheimer’s diseased brains.
Can cardiovascular disease and Alzheimer’s disease be connected? Researchers are still working to discover the underlying mechanisms, but it appears to be something worth investigating further. There are very similar components of the progression of both cardiovascular disease and Alzheimer’s disease—for instance, they share a common risk factor: oral biofilm.
The oral bacteria that most show up most often in both cardiovascular disease and Alzheimer’s disease are Porphyromonas gingivalis and Treponema denticola:
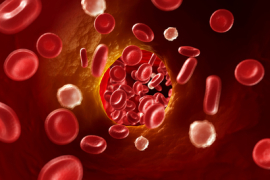
- P. gingivalis has been shown to play a role in the progression of macrophages into foam cells in the coronary arteries.
- Oral treponemes are beginning to be looked at as causal of Alzheimer’s disease.
- Research released earlier this year shows us that the two bacteria seem to play off each other and may even increase both activity and severity of their effects.
- P. gingivalis lipopolysaccharides are often found at the site of destruction where the treponemes are doing their damage in the brain.
Research has well established that oral pathogens play an important role in the progression of disease in the thickening of the coronary arteries, plaque formation, and also in the progression of Alzheimer’s disease. This latest study shows us that thickening of those coronary arteries and the inflammatory effects are significantly correlated with the presence of beta amyloid plaques in the brain.
Inflammation plays a role—possibly causal—in most inflammatory disease, including heart disease and Alzheimer’s disease. Oral inflammation, the most common form of inflammation in humans, is increasingly being recognized as a contributor to the inflammatory cascade that leads to these diseases.
We are finding that it does not take severe gum disease—bleeding, puffy gums, for instance—in order for oral inflammation to have an effect on systemic inflammation and disease. Even the smallest microbial burden can have a huge impact on systemic disease, especially when you take into account genetic variations and lifestyle factors (e.g. stress, diet, and physical activity).
Sources:
More Research Links Poor Heart Health With Alzheimer’s Risk
Arterial Stiffness and β-Amyloid Progression in Nondemented Elderly Adults