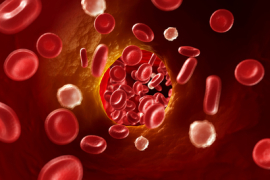
Certain periodontal bacteria can make their way into the brain, according to a recent collaborative study by University of Central Lancastershire and University of Florida researchers. And there is evidence that these bacteria lay the groundwork for Alzheimer’s disease.
Researchers examined mice models that had been orally infected with both mono- and poly-microbial bacterial loads, then examined their brains after a period of 12 or 24 weeks. They found bacterial DNA in nearly all of the experimental group’s brains, indicating that bacteria do, in fact, translocate to the brain during the infectious process.
This study was first presented at the German Borreliosis Society’s annual conference in Erfurt, Germany, where biofilm experts from around the world convened to discuss the impact of biofilms on overall health.
“It’s early work. We’ve definitely shown that periodontal bacteria are getting access to brains in humans,” said Dr. StJohn Crean, a researcher on the project.
Worth mentioning in this study is that the mice used were all genetically APO-E null. APO-E null mice are often used in research because they mimic humans with APO-E abnormalities in humans. APO-E null mice (and humans with APO-E abnormalities) have been found to be more likely to have atherosclerosis, Alzheimer’s disease, and a shorter lifespan.
While the researcher team found bacterial DNA in the brains from both the mono- and poly-microbial experimental groups, P. gingivalis was by far the most prevalent. Interestingly, P. gingivalis didn’t seem to excite a huge amount of cytokine activity in these cells, yet the Treponemes and Tannerellas did. Dr. Crean said that this was encouraging evidence that “P. gingivalis is the first one in, and the rest of the real hitters will arrive later.” This looks like P. gingivalis is the first one in and the rest of the likes of Treponemes and Tannerellas arrive later.
This study is one in a long line of research from Dr. Crean’s team, which is exploring the effects of oral bacteria on the development and progression of Alzheimer’s disease.
From their research, it’s starting to look like P. gingivalis is part of the attack complex that enters first, and the other pathogens follow. There may be evidence that they’re not only there, but they may well be activating prime glial cells, which goes on to damage the neuronal cells.
They also showed that neurons—the synaptic important cells—were being covered in activation fragments complement (part of the inflammation process) in the absence of beta amyloid, which supports the hypothesis that P. gingivalis disseminates in the brain and can initiate the brain’s own immune response as opposed to being a result of beta-amyloids.
The presence of amyloid proteins in Alzheimer’s diseased brains has long been studied as a cause of the degeneration of brain tissue, but a surge in research on the role of pathogens has opened up a new discussion into the possible causes of this degenerative disease.