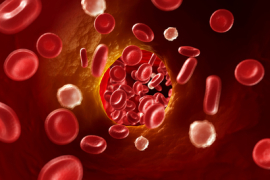
The oral microbiome contains a diverse range of bacterial species even in the healthiest of situations, so it is not surprising that most oral infections likewise contain more than one type of pathogen.
A recent study published in the Archives of Oral Biology demonstrated that the presence and co-infection of Fusobacterium nucleatum enables other pathogens to do more damage than they would ordinarily be able to do.
F. nucleatum enhanced the ability of both P. gingivalis and A. actinomycetemcomitans to adhere to and invade host cells. Likewise, P. gingivalis and A. actinomycetemcomitans disrupted the inflammatory response to F. nucleatum.
All these pathogens are invasive, and they have demonstrated time and time again that they can manipulate the immune system. P. gingivalis has been shown to turn white blood cells into carriers for itself, quite literally sabotaging the body’s immune response. F. nucleatum appears to block the immune system from attacking colon cancer cells.
And when these bacteria get together, they can exacerbate the harm than any one of them could do alone.
When we keep in mind that all of this could be happening while a person exhibits no traditional signs of periodontal disease (a person can have healthy looking gums but still have a very high bioburden), it becomes ever more important that we define periodontal disease by pathogens. With tools to help us quantify microbial burden, we can more accurately and effectively address the risks at hand.